Update: Changes in prior authorization for Blue Cross NC outpatient therapy requests now effective December 1
Update November 1, 2024: On August 29, 2024, Blue Cross NC issued a provider notice announcing the transition of medical necessity review of outpatient therapy services for Commercial Fully Insured members to Carelon effective November 1, 2024.
Due to a technical issue identified on October 21 affecting providers’ access to the Carelon portal, the previously announced effective date for this program has been delayed one month. The new effective date is December 1, 2024.
Carelon Portal Access
Providers attempting to enter a request on the Carelon portal for the Rehabilitation Program may encounter one of the following scenarios:
1. The provider can submit their request with no issue (most providers should be in this category).
2. The provider enters their request and is directed to enter their demographic information. This information is required to move forward with the request.
3. The provider enters their request and the below “Apologies” page appears once member information is entered and the “Rehabilitation” icon is selected.
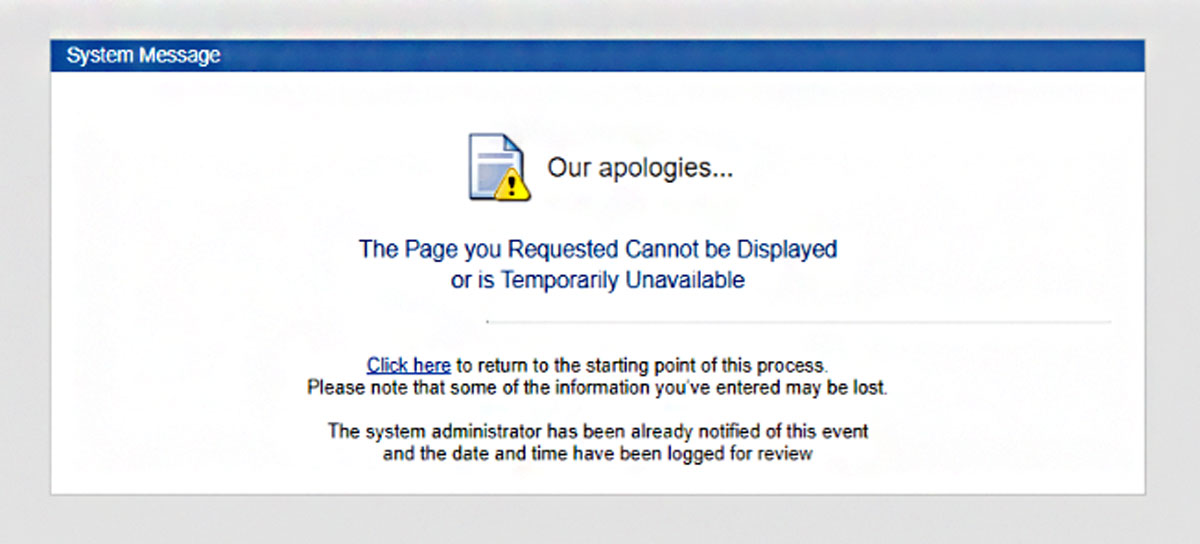
If you see the "Apologies" page after entering the member's information and selecting the "Rehabilitation" icon, you will need to follow these steps to fix the issue.
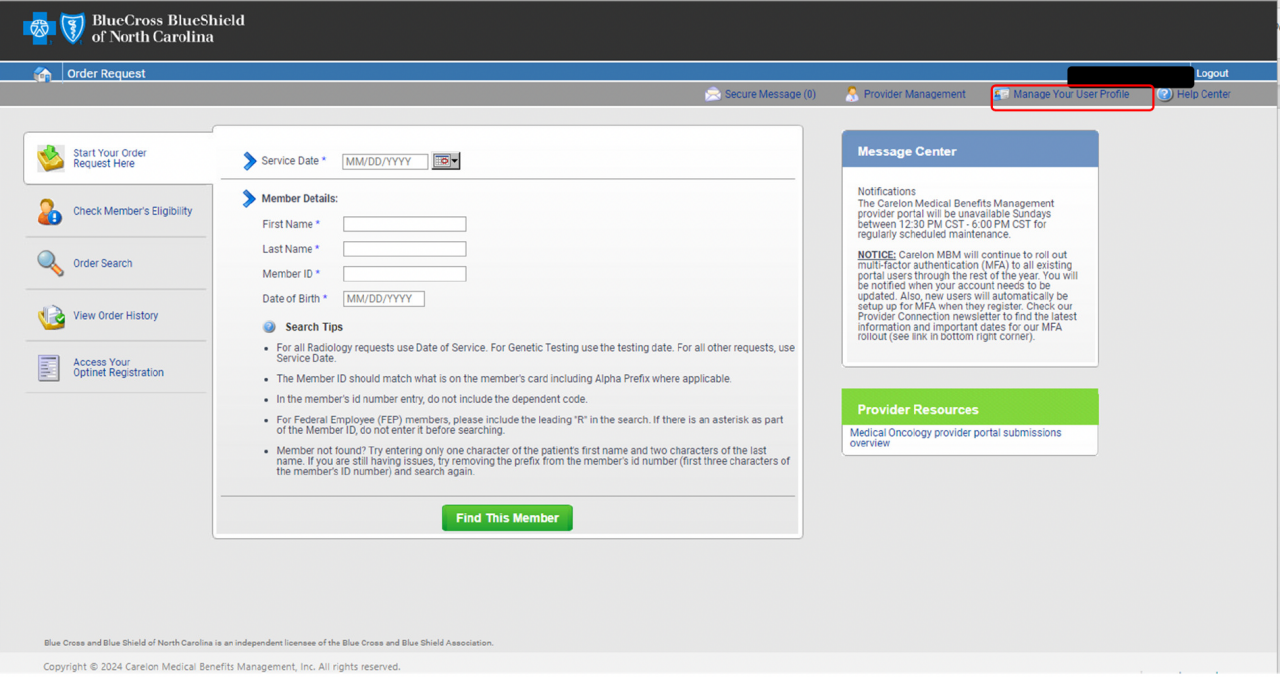
1. In the Carelon portal, select “Manage Your User Profile.”
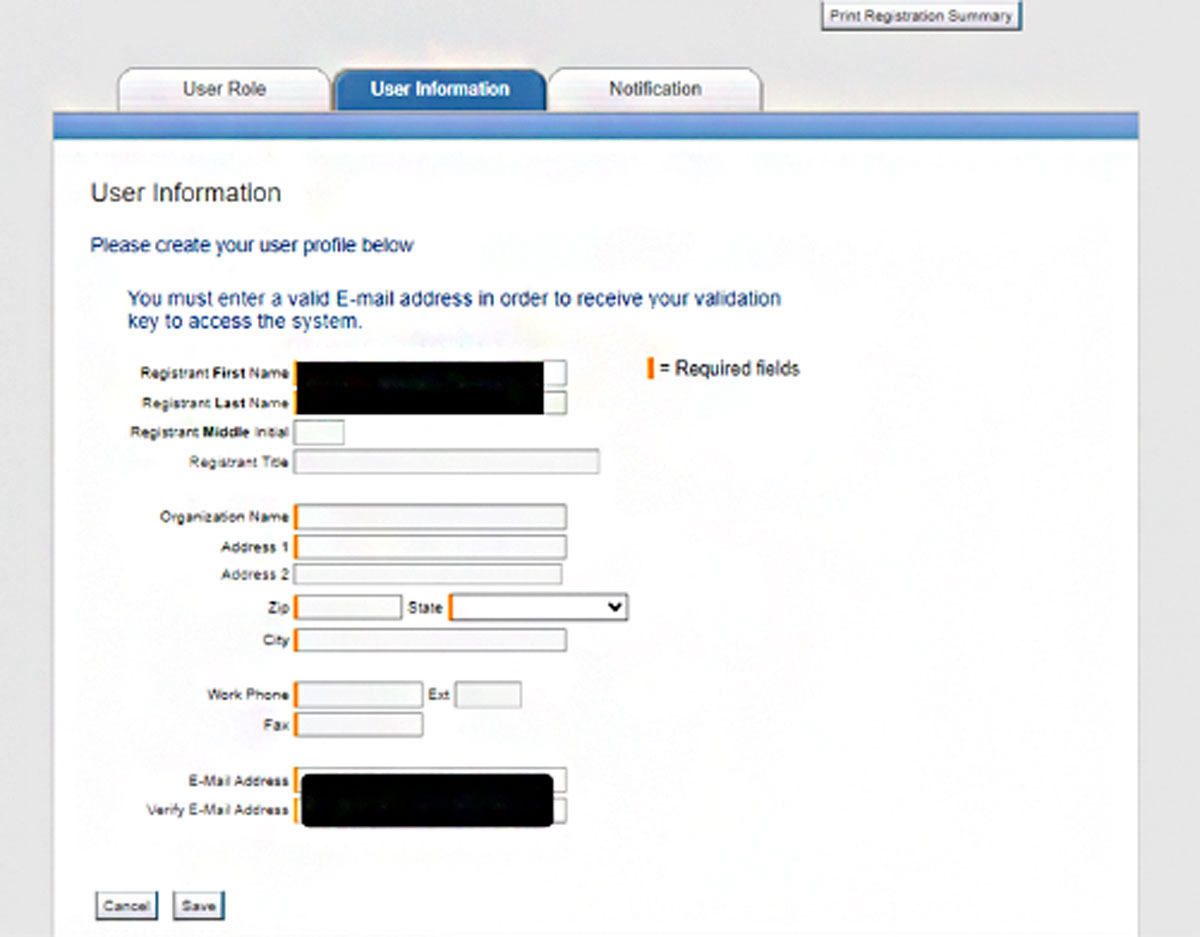
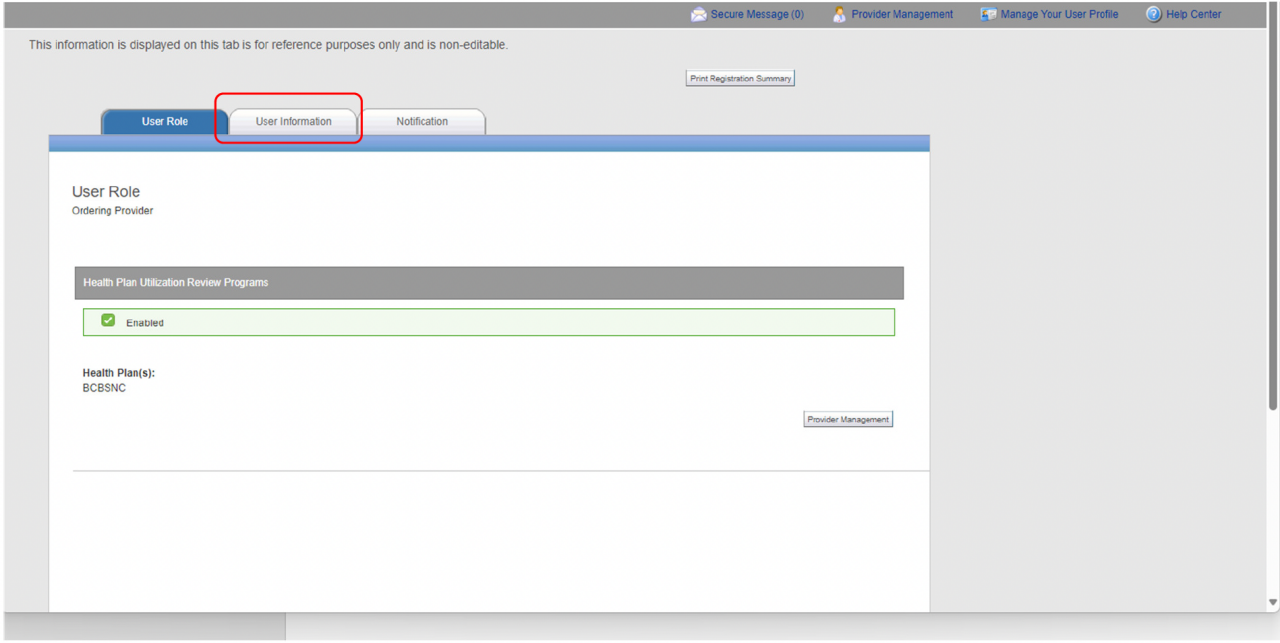
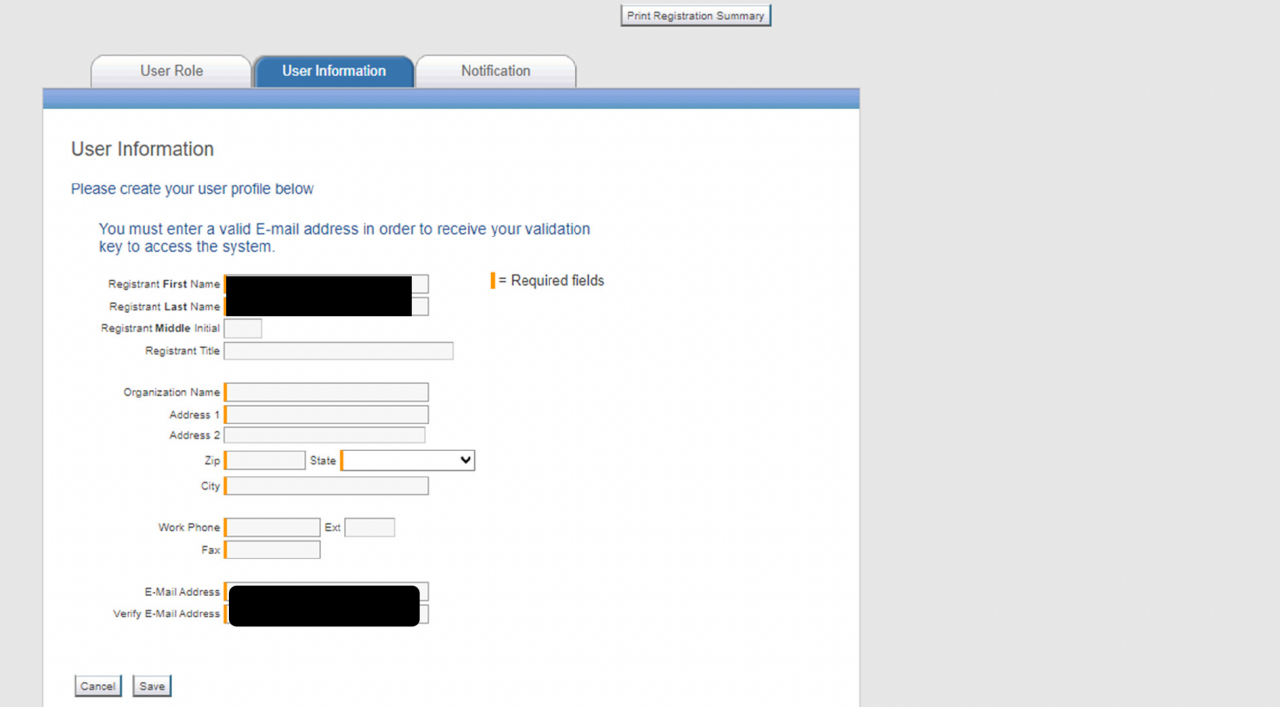
2. Select the “User Information" tab.
3. Enter your information in the orange required fields and select "Save."
4. Select the “Home” icon to return to the home page and submit a request.
Providers who have already obtained an authorization extending beyond the December 1 effective date do not need to request a new authorization for dates that are included in the previously submitted request. However, any dates outside of that period or any new service codes not included in the original authorization will require a new request. Therapy prior authorization requests through Carelon cannot be submitted more than 30 days in advance of the requested service date.
We appreciate your patience as we work to ensure a successful launch of this program.
For questions, please contact the Provider Service line located on the back of the member’s identification card.
Blue Cross and Blue Shield of North Carolina does not discriminate on the basis of race, color, national origin, sex, age or disability in its health programs and activities. Learn more about our non-discrimination policy and no-cost services available to you.
Information in other languages: Español 中文 Tiếng Việt 한국어 Français العَرَبِيَّة Hmoob ру́сский Tagalog ગુજરાતી ភាសាខ្មែរ Deutsch हिन्दी ລາວ 日本語
© 2025 Blue Cross and Blue Shield of North Carolina. ®, SM Marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield plans. All other marks and names are property of their respective owners. Blue Cross and Blue Shield of North Carolina is an independent licensee of the Blue Cross and Blue Shield Association.
